Information, Tests and Solutions to Improve
Your Health and Water Quality |
Malondialdehyde levels are used in this research as a determining factor of free radical mediated cell injury in burn trauma.
ifts that, in turn, reduce cardiac output and tissue perfusion. Treatment approaches to major burn injury include administration of crystalloid solutions to correct hypovolemia and to restore peripheral perfusion. While this aggressive postburn volume replacement increases oxygen delivery to previously ischemic tissue, this restoration of oxygen delivery is thought to initiate a series of deleterious events that exacerbate ischemia-related tissue injury. While persistent hypoperfusion after burn trauma would produce cell death, volume resuscitation may exacerbate the tissue injury that occurred during low flow state. It is clear that after burn trauma, tissue adenosine triphosphate (ATP) levels gradually fall, and increased adenosine monophosphate (AMP) is converted to hypoxanthine, providing substrate for xanthine oxidase. These complicated reactions produce hydrogen peroxide and superoxide, clearly recognized deleterious free radicals. In addition to xanthine oxidase related free radical generation in burn trauma, adherent-activated neutrophils produce additional free radicals. Enhanced free radical production is paralleled by impaired antioxidant mechanisms; as indicated by burn-related decreases in superoxide dismutase, catalase, glutathione, alpha tocopherol, and ascorbic acid levels. Burn related upregulation of inducible nitric oxide synthase (iNOS) may produce peripheral vasodilatation, upregulate the transcription factor nuclear factor kappa B (NF-kappaB), and promote transcription and translation of numerous inflammatory cytokines. NO may also interact with the superoxide radical to yield peroxynitrite, a highly reactive mediator of tissue injury. Free radical mediated cell injury has been supported by postburn increases in systemic and tissue levels of lipid peroxidation products such as conjugated dienes, thiobarbituric acid reaction products, or malondialdehyde ( MDA ) levels Antioxidant therapy in burn therapy (ascorbic acid, glutathione, N-acetyl-L-cysteine, or vitamins A, E, and C alone or in combination) have been shown to reduce burn and burn/sepsis mediated mortality, to attenuate changes in cellular energetics, to protect microvascular circulation, reduce tissue lipid peroxidation, improve cardiac output, and to reduce the volume of required fluid resuscitation. Antioxidant vitamin therapy with fluid resuscitation has also been shown to prevent burn related cardiac NF-kappaB nuclear migration, to inhibit cardiomyocyte secretion of TNF-alpha , IL -1beta, and IL-6, and to improve cardiac contractile function. These data collectively support the hypothesis that cellular oxidative stress is a critical step in burn-mediated injury, and suggest that antioxidant strategies designed to either inhibit free radical formation ( malondialdehyde ) or to scavage free radicals may provide organ protection in patients with burn injury. Return from Free Radical Reference 1 Malondialdehyde |
You are here: Home Page > Free Radical Test > Free Radical Laboratory Validation 1 > Free Radical Reference 1
Natural Care Solution:
Helping People Improve Their Health Naturally Since
1998
|
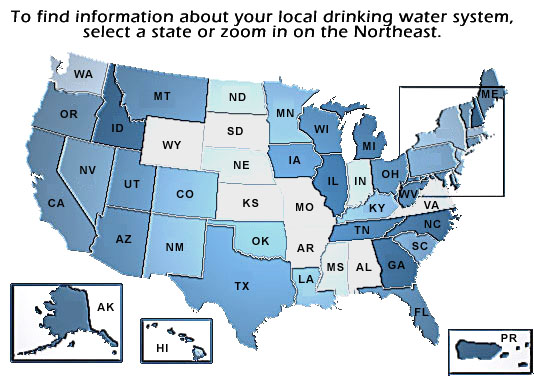
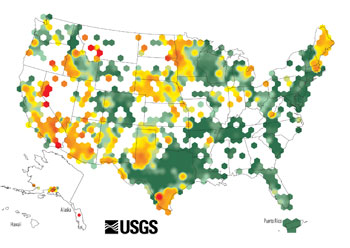
Quality Water Testing and Analysis for Residential and Commercial Water Sources
My Mission
Provide you with accurate information, economical and
effective tests
and products to evaluate your body and water for toxic metals and remove them if
necessary.
Keith D. Bishop
Clinical Nutritionist
B.Sc. Pharmacy
Health
Coach©

|
*These statements have not been evaluated by the Food and Drug Administration. These products are
not intended to diagnose, treat, cure or prevent any disease.
The information and contents of this website are based upon government, medical,
university and health industry research information.
Consult with your physician or a qualified health care provider before making any changes in your medical or
treatment program.
Please let us know if you have problems viewing anything or ordering on this page:
Thank you for visiting www.ToxicWaterSolution.com! If you find this information helpful or
interesting please send a link to your family and friends.
Copyright © 2007-2016 Natural Care Solution, LLC Keith D. Bishop, Clinical Nutritionist, B.Sc. Pharmacy
 1. Horton, Jureta W.
1. Horton, Jureta W.